While the mortality rate for COVID-191 varies around the world (in large part due to variations in testing), one trend is clear: The infection disproportionately affects the elderly, with those over the age of 75 making up the bulk of the deaths.
COVID-19 Outcomes Tied to Age
Looking at provisional data2 from the U.S. Centers for Disease Control and Prevention, you can see a clear and dramatic increase in deaths for each older age group.
For young people, especially children, the risk of death is negligible. (Even so, more elderly die from pneumonia that is unrelated to COVID-19. The statistics separate out COVID-19 cases, pneumonia only, and pneumonia with concurrent COVID-19 infection.3)
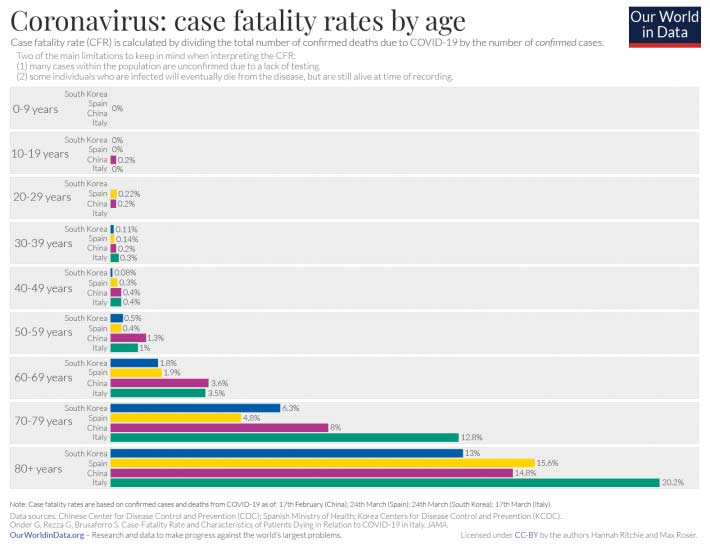
The exact same age-dependent trend is seen in other countries, four examples of which are included in the OurWorldInData.org’s graph below.4 As noted in a May 29, 2020, review5 in the journal Aging, “Adults over 65 years of age represent 80% of hospitalizations and have a 23-fold greater risk of death than those under 65.”
Below is a graph created by the Minnesota Department of Health, published by Twin Cities Pioneer Press6 June 1, 2020, showing the same kind of age-dependent mortality curve.

Underlying Conditions Are a Primary Risk Factor
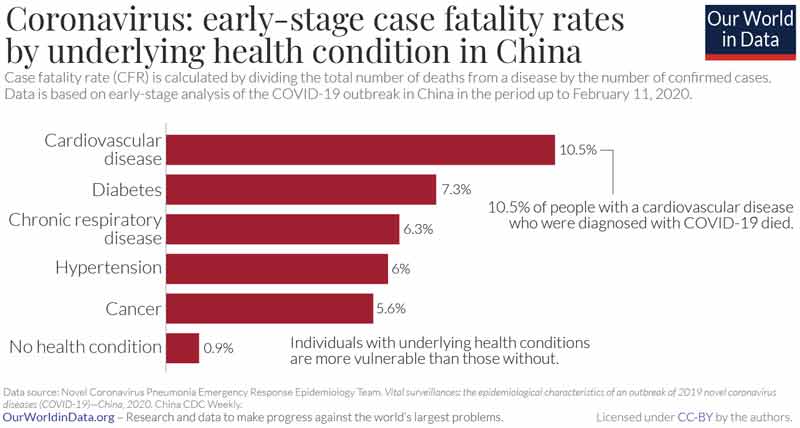
In addition to age, underlying health conditions (so-called comorbidities) are a primary risk factor that raises your risk of death from COVID-19. Not surprisingly, the elderly tend to have more underlying conditions. Very few people who have no underlying health conditions at all end up dying from this infection.
Below is an Our World in Data graph showing the breakdown of comorbidities found in Chinese patients, as of February 11, 2020.7
Another graph from the Minnesota Department of Health, (again, published by Twin Cities Pioneer Press8) reveals a different picture of prevailing comorbidities, yet the trend itself is clear: A vast majority of those who die have underlying conditions that make them more susceptible to severe infection and death.

In the case of Minnesota, 97% of COVID-19-related deaths have occurred in those “already fighting serious illness before they were infected.“9 The average age of those who have died is 82. Meanwhile, the medial age of Minnesotans with known COVID-19 infection is 42.
Just like in other areas, more than 80% of deaths occurred in nursing homes, assisted living facilities and live-in rehab centers, and there are logical reasons for this. More than 90% of residents of these centers have at least one chronic disease and more than 70% have two conditions, which in turn can weaken their immune systems.10 They also live in close quarters and share staff, which facilitates the spread of pathogens.
Italy and certain states in the U.S. — most notably New York, which has the highest COVID-19 death rate in the world — made the grave error of sending COVID-19 infected patients into nursing homes.
In light of what we currently know about the transmission, this was one of the most catastrophic and negligent government decisions that likely caused far more deaths than the lockdown prevented.
Rather than calling for the total lockdown of healthy and low-risk populations, why did health and government officials not simply call for the protection and isolation of the elderly?
According to a May 15, 2020, report by the University of Michigan,11 nursing home residents and workers account for about one-third of all COVID-19 deaths in the U.S. Another report12 in The Guardian has pointed out that up to 20% of hospitalized COVID-19 patients actually caught it in the hospital while being treated for another ailment.
If 20% of people catch the disease at the hospital and 33% of deaths happen in nursing homes, just how much of the entire disease burden is a result of the health care system alone?
Biological Differences Help Explain Age-Related Morbidity
According to the outstanding May 29, 2020, review by David Sinclair on the molecular biology of COVID-1913 mentioned earlier, “Comorbidities such as cardiovascular disease, diabetes and obesity increase the chances of fatal disease, but they alone do not explain why age is an independent risk factor.”
If that’s so, then what else might account for the radical discrepancy in mortality? In his excellent review, Sinclair discusses the “molecular differences between young, middle-aged and older people that may explain why COVID-19 is a mild illness in some but life-threatening in others.” If you have any interest in this topic I would strongly recommend reading this paper.
Importantly, Sinclair points out that inhibiting the virus is not enough in and of itself. One must also restore the patient’s ability to fight the infection and upregulate their immune responses to avoid an overreaction. This is done by many strategies I have previously discussed such as exercise, time-restricted eating and NAD+ optimization.
The Aging Immune System
Topping the list of additional factors that make the elderly more susceptible to dying is an aging immune system — both the innate and adaptive arms. As noted by Sinclair:14
“For the immune system to effectively suppress then eliminate SARS-CoV-2, it must perform four main tasks: 1) recognize, 2) alert, 3) destroy and 4) clear. Each of these mechanisms are known to be dysfunctional and increasingly heterogeneous in older people.”
During aging, your immune system undergoes a gradual decline in function known as immunosenescence, which inhibits your body’s ability to recognize, alert and clear pathogens. Aging also increases systemic inflammation, known as inflammaging, thanks to an overactive yet ineffective alert system. According to Sinclair:
“An abundance of recent data describing the pathology and molecular changes in COVID-19 patients points to both immunosenescence and inflammaging as major drivers of the high mortality rates in older patients.
The inability of [alveolar macrophages] AMs in older individuals to recognize viral particles and convert to a pro-inflammatory state likely accelerates COVID-19 in its early stages, whereas in its advanced stages, AMs are likely to be responsible for the excessive lung damage.”
Sinclair also addresses the impact an aging innate immune system has on vaccination efficacy, noting that:
“In the aged, immune responses to vaccination are also often weak or defective whereas autoimmunity increases. Therefore, in designing vaccines against SARS-CoV-2, it will be important to consider that older people may not respond as well to vaccines as young people.”
Vascular Inflammation Is a Risk Factor
While we have all heard of the cytokine storm, what is even more predictive of death is an increase in the fibrin degradation product D-dimer that is released from blood clots in the microvasculature and is highly predictive of disseminated intravascular coagulation (DIC). The elderly have naturally higher levels of D-dimer, which appears to be a “key indicator for the severity of late-stage COVID-19,” the Sinclair states.15
In the elderly, elevated levels are thought to be due to higher basal levels of vascular inflammation associated with cardiovascular disease, and this, the authors say, “could predispose patients to severe COVID-19.” Similarly, the elderly tend to have higher levels of NLRP3 inflammasomes, which appear to be a key culprit involved in cytokine storms. According to Sinclair:
“In older individuals, NLRP3 may be poised for hyperactivation by SARS-CoV-2 antigens. NLRP3 activity is under the direct control of sirtuin 2 (SIRT2), a member of the NAD+-dependent sirtuin family of deacetylases.
During aging, NAD+ levels decline, reducing the activity of the sirtuins. Old mice … have decreased glucose tolerance and increased insulin resistance. This decline, exacerbated by COVID-19, might promote hyperactivation of NLRP3 and the trigger [for] cytokine storms in COVID-19 patients.”
Higher NAD+ Level May Be Protective
Importantly, he points out that maintaining optimal NAD+ levels may therefore alleviate COVID-19 symptoms. This theory is further supported by recent data showing “SARS-CoV-2 proteins … deplete NAD+,” and the fact that NAD+ precursors are known to inhibit inflammation.
Helpful strategies to achieve that include taking NAD precursors such as nontimed-release niacin, lowering your sugar intake (as excess blood glucose lowers NAD+), cyclical nutritional ketosis, and/or taking glycine or collagen.
Other Factors at Play
Other factors that predispose the elderly to severe infection and death include epigenetic changes that occur with age, specifically:
- The dysregulation of the epigenome
- Excessive calorie intake
- Changes in glycosylation (the enzymatic process by which glycans, a type of carbohydrate, are covalently attached to proteins or fats on the cell surface or in the bloodstream)
Sinclair points out that metformin, a glucose-lowering drug that inhibits the mTOR pathway, “has been suggested as a possible drug to combat severe SARS-CoV-2 infection in older people.”
Metformin also has antiviral effects and helps improve mitochondrial metabolism, decrease inflammatory cytokines, decrease cellular senescence and protect against genomic instability, Sinclair notes.
The following illustrations from his review16 summarize the biological mechanisms that determine your COVID-19 susceptibility and subsequent risk of death.


Vitamin D Is a Simple Strategy That Can Save Lives
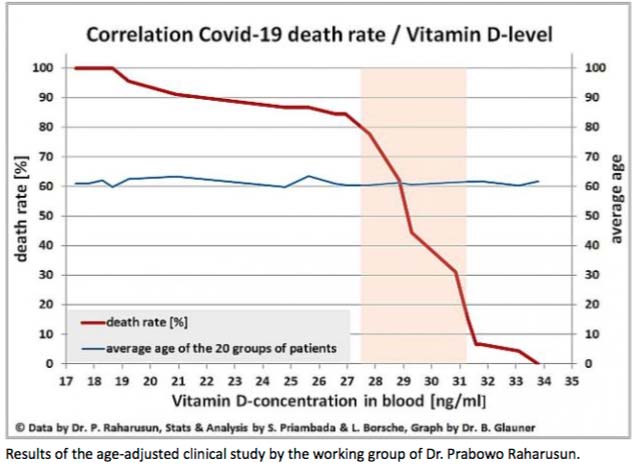
The elderly also tend to have low vitamin D levels, and vitamin D deficiency is another trend that several researchers have now identified as an underlying factor that significantly impacts COVID-19 severity and mortality. I discuss this in “Vitamin D Is Directly Correlated to COVID-19 Outcome.”
The following graph is from a May 18, 2020, letter17 to the Federal Chancellor of Germany, Angela Merkel, from retired biochemist Bernd Glauner and Lorenz Borsche, in which they highlight studies18 showing a clear correlation between COVID-19 mortality and vitamin D levels.
It’s important to note that experts are already warning SARS-CoV-2 may reemerge in the fall when temperatures and humidity levels drop, thereby increasing the virus’ transmissibility.
To improve your immune function and lower your risk of viral infections, you’ll want to raise your vitamin D to a level between 60 nanograms per milliliter (ng/mL) and 80 ng/mL by fall. In Europe, the measurements you’re looking for are 150 nanomoles per liter (nmol/L) and 200 nmol/L. Optimizing your vitamin D is particularly important if you are older or have darker skin.
One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit, either alone or in combination with the omega-3 test. This is done in the convenience of your home.
To make sure your vitamin D level and immune system function are optimized, follow these three steps:
1. Measure your vitamin D level — Once you know what your blood level is, you can assess the dose needed to maintain or improve your level. The easiest way to raise your level is by getting regular, safe sun exposure, but if you’re very dark-skinned, you may need to spend about 1.5 hours a day in the sun to have any noticeable effect.
Those with very light skin may only need 15 minutes a day, which is far easier to achieve. Still, they too will typically struggle to maintain ideal levels during the winter. So, depending on your situation, you may need to use an oral vitamin D3 supplement. The next question then becomes, how much do you need?
2. Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5. To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, consider using the DMinder app.19
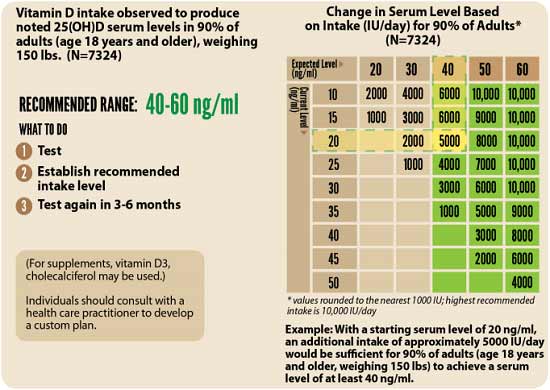
3. Retest in three to six months — Lastly, you’ll need to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.
Not only will optimizing your vitamin D be an important strategy for you and your family, but it would be really helpful to start thinking about your community as well. I am in the process of writing an even more comprehensive and detailed report on vitamin D in the prevention of COVID-19 and I hope to enlist ALL of you to talk to your friends and family and get them on board to get their vitamin levels optimized.
If you can, speak to pastors in churches with large congregations of people of color and help them start a program getting people on vitamin D, and if you have a family member or know anyone who is in an assisted living facility, meet with the director of the program and encourage them to get everyone tested or at least start them on vitamin D.
from Articles https://ift.tt/3hl5zWJ
via IFTTT








0 comments:
Post a Comment