According to a British observational study1 posted July 6, 2020, on the preprint server medRxiv, ultraviolet (UV) radiation exposure appears to lower COVID-19 mortality rates.
As reported by News Medical Life Sciences,2 environmental factors such as temperature, humidity and UV irradiation are known to play a role in other infectious diseases, including seasonal influenza, so it shouldn’t come as a surprise that SARS-CoV-2 — the virus responsible for COVID-19 — can be affected in a similar manner.
UV Radiation Lowers COVID-19 Mortality
I’ve written extensively about the importance of vitamin D and its influence on COVID-19 specifically, but this research suggests there are other benefits to sun exposure besides vitamin D production.
The researchers looked at UVA measures and COVID-19 death statistics in 2,474 U.S. counties, 6,755 Italian municipalities and 6,274 areas in England between the months of January and April 2020, which is when vitamin D production due to low sun exposure tend to be minimal. According to the authors:3
“Our fully adjusted model showed an inverse correlation between UVA and COVID-19 mortality with a Mortality Risk Ratio (MRR) of 0.73 … per 100KJ/m2 increase UVA in the USA, 0.81 … in Italy and 0.51 … in England. Pooled MRR was 0.68 …
This represents a halving of the average risk of death across the lower and narrower range of UVA experienced across England and across the higher and wider range across Italy and the USA …
Our analysis suggests that higher ambient UVA exposure is associated with lower COVID-19 specific mortality. This effect was independent of temperature and UV within the vitamin D action spectrum.
Relatively higher UVA, across a country experiencing lower average levels of UVA during and immediately preceding the pandemic (England), is associated with greater falls in mortality risk compared to countries (Italy and the USA) with a higher average level suggesting an exposure tolerance effect …
We have been able to show a possible benefit from UV at wavelengths that do not cause synthesis of vitamin D. this suggests that explanations for seasonal and geographic variations in COVID-19 prevalence need to consider mechanisms other than just vitamin D.”
Mechanisms of Action
The researchers hypothesize UV exposure “may have a direct effect on the viability of SARS-CoV-2 virus in airborne droplets,” as well as the virus’ ability to stay viable on various surfaces, thus reducing overall infection rates and lowering the initial inoculation load in those infected, which in turn might reduce the risk of severe illness.
Another mechanism of action may involve nitric oxide. UVA radiation triggers the release of nitric oxide in your skin, mobilizing it into your circulation. This lowers blood pressure by causing your blood vessels to expand. This, the researchers say, is one important metabolic benefit of UV exposure that does not involve vitamin D.
“As cardio-metabolic disease and possibly hypertension increase the risk of death from COVID-19, any UV driven improvements in these risk factors would be expected to reduce mortality,” the researchers note.
What’s more, nitric oxide may help mitigate the endothelial damage seen in severe COVID-19 infection that leads to organ failure. While not mentioned in this study, nitric oxide also improves your immune function, thins your blood and decreases blood viscosity, which in turn decreases platelet aggregation. As such, nitric oxide helps reduce your risk of developing a life-threatening blood clot.
Previous research has also found nitric oxide inhibits replication of the SARS virus (SARS-CoV), and the researchers hypothesize that, since the spike proteins of the two viruses are similar, nitric oxide may have a similar effect on SARS-CoV-2. If correct, this could be yet another mechanism of action by which nitric oxide helps reduce disease transmission and severity.
So, to summarize, not only does exposure to sunlight lower COVID-19 mortality, but just about any strategy that boosts nitric oxide production may also have a similar effect. Examples of such strategies include the Nitric Oxide Dump workout and consuming nitrate-rich foods such as beetroot juice, arugula and cilantro.
Are Stay-At-Home Orders Increasing COVID-19 Mortality?
In related news, another study4 posted on medRxiv, July 2, 2020, asks whether lockdown orders might do more harm than good by decreasing the protective role of UVB radiation — the kind that triggers vitamin D production in your skin — which has also been shown to lower COVID-19 mortality rates. As noted by the authors:
“Recent studies indicate that measures such as lockdowns may have slowed down the growth of COVID-19. However, in addition to substantial economic and social costs, these measures also limit the exposure to Ultraviolet-B radiation (UVB).
Emerging observational evidence indicate the protective role of UVB and vitamin D in reducing the severity and mortality of COVID-19 … In this observational study, we empirically outline the independent protective roles of lockdown and UVB exposure as measured by ultraviolet index (UVI), whilst also examining whether the severity of lockdown is associated with a reduction in the protective role.”
According to their calculations, mortality rates could have been reduced by an average of 21% had lockdown orders been accompanied by instructions to get regular sun exposure.
Vitamin D Lowers All COVID-19 Related Risks
As reviewed in several previous articles, vitamin D appears to impact virtually all COVID-19 related risks, including your risk of testing positive for active infection, disease severity and your risk of death. For example:
|
Research5 posted on the preprint server medRxiv, May 13, 2020, found low vitamin D status at the time of COVID-19 testing was a risk factor for a positive result. Compared to those with sufficient vitamin D levels, those with deficient levels were nearly twice as likely to test positive for COVID-19 (21.6% versus 12.2%). |
|
A study6 from the Philippines found that for each standard deviation increase in serum vitamin D, the odds of experiencing only mild disease rather than severe illness was 7.94 times greater, and the odds of having a mild clinical outcome rather than a critical outcome was 19.61 times greater. |
|
Research7,8 posted on the preprint server MedRxiv June 10, 2020, reports a combination of vitamin D3, magnesium and B12 inhibited the progression of COVID-19 in patients over the age of 50, resulting in “a significant reduction in proportion of patients with clinical deterioration requiring oxygen support and/or intensive care support.” |
|
A study9 from Indonesia found COVID-19 patients with a vitamin D level between 20 ng/mL (50 nmol/L) and 30 ng/mL (75 nmol/L) had a sevenfold higher risk of death than those with a level above 30 ng/mL. Having a level below 20 ng/mL was associated with a 12 times higher risk of death. |
|
A study10 that looked at data from 20 European countries found that “the probability of developing COVID-19, and of dying from it, is negatively correlated with mean population vitamin D status, with both probabilities reaching zero above about 75 nmol/L,” (30 ng/mL). |
|
A paper11,12 posted on the preprint portal medRxiv May 18, 2020, found a strong correlation between severe vitamin D deficiency and higher mortality rates in countries across the globe. The researchers attribute this to a connection between low vitamin D and high risk for cytokine storms. The analysis suggests higher vitamin D levels among the general population could cut mortality in half by reducing complications.13 |
Higher Vitamin D Lowers All-Cause Mortality Risk
COVID-19 certainly isn’t the only disease influenced by vitamin D. As noted in a study14 published July 4, 2020, in the Journal of Clinical Endocrinology and Metabolism, higher vitamin D levels are “non-linearly linked to lower risk of all-cause, [cardiovascular disease] CVD, and cancer mortality.”
Interestingly enough, this study found the risk for CVD and all-cause deaths tapered off at a vitamin D level of just 24 ng/mL (60 nmol/L). Cancer deaths leveled off at a mere18 ng/mL (45 nmol/L).
This is surprisingly low, considering large-scale studies suggest the cutoff for optimal cancer protection is around 40 ng/mL (100 nmol/L), with a level of 60 ng/mL to 80 ng/mL (150 nmol/L to 200 nmol/L) being ideal for health and disease prevention. You can learn more about this in “For Optimal Health, Make Sure You Have a Vitamin D Level of 60 ng/mL.”
Magnesium Optimizes Vitamin D Supplementation
According to a scientific review15,16 published in 2018, as many as 50% of Americans taking vitamin D supplements may not get significant benefit as the vitamin D simply gets stored in its inactive form, and the reason for this is because they have insufficient magnesium levels, and magnesium is required in the conversion of vitamin D into its active form.
Research17 published in 2013 also highlighted this issue, concluding that higher magnesium intake helps reduce your risk of vitamin D deficiency by activating more of it.
More recently, research18 by GrassrootsHealth reveals you need 146% more vitamin D to achieve a blood level of 40 ng/ml (100 nmol/L) if you do not take supplemental magnesium, compared to taking your vitamin D with at least 400 mg of magnesium per day.
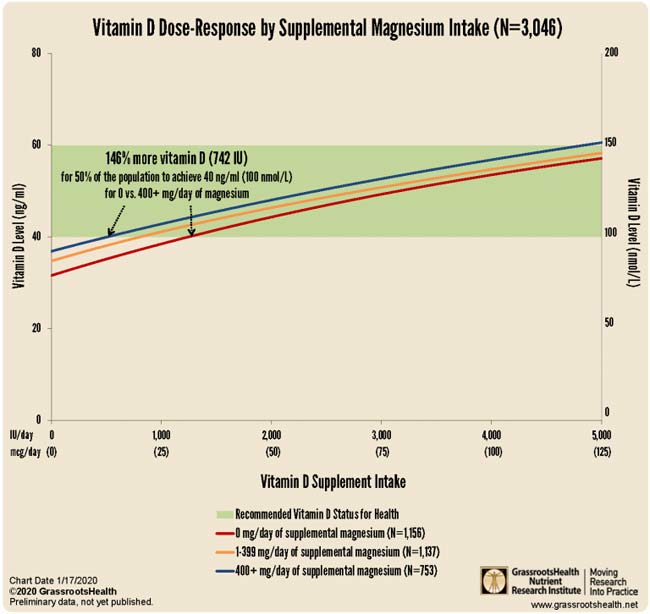
You can cut your need for oral vitamin D even further — by as much as 244% — by taking it concurrently with both magnesium and vitamin K2, as reported in “Magnesium and K2 Optimize Your Vitamin D Supplementation.”
Optimize Your Vitamin D Level to Minimize COVID-19 Risks
While oral vitamin D supplementation may be a good idea for most people, it’s important to remember to get your vitamin D level tested first. The reason for this is because you cannot rely on blanket dosing recommendations. The crucial factor here is your blood level, not the dose, as the dose you need is dependent on several individual factors, including your baseline blood level.
I recently published two vitamin D reports, a comprehensive scientific review and a shorter summary, in which I detail vitamin D’s mechanisms of action and how to ensure optimal levels. I recommend downloading and sharing those reports with everyone you know.

Here’s a condensed summary of the key steps to optimizing your vitamin D:
1. First, measure your vitamin D level — One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit. You also have the option of testing vitamin D in conjunction with magnesium and omega-3.
Once you know what your blood level is, you can assess the dose needed to maintain or improve your level. If you cannot get enough vitamin D from the sun (you can use the DMinder app19 to see how much vitamin D your body can make depending on your location and other individual factors), then you’ll need an oral supplement.
2. Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5.
To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, use the DMinder app.20 Remember, you won’t need as much oral vitamin D if you also take magnesium and vitamin K2, as discussed above.
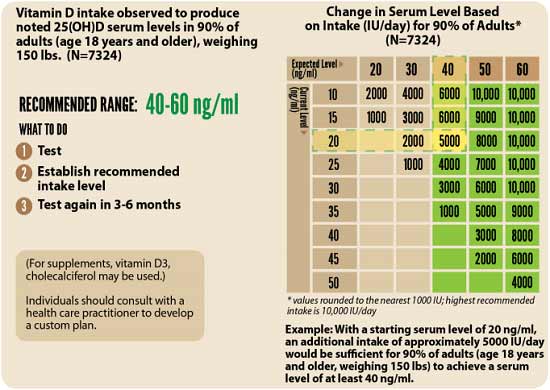
3. Retest in three to six months — Lastly, you’ll need to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.
from Articles https://ift.tt/3fMLN5p
via IFTTT








0 comments:
Post a Comment